Learning Objectives
- Define and differentiate between vaccination and the resulting immunization.
- Explain how the adaptive immune system works in response to a vaccination to create immunity in the host, including the names of the immune system cells and how they interact with each other.
- Recognize implications of decreased vaccination rates.
- Know the different types of allergic response.
- Explain how the immune system can attack own body cells and give some examples.
What are vaccines and how do they work?
[From Khan Academy]
Because the adaptive immune system can learn and remember specific pathogens, it can provide long-lasting defense and protection against recurrent infections. When the adaptive immune system is exposed to a new threat, the specifics of the antigen are memorized so we are prevented from getting the disease again. The concept of immune memory is due to the body’s ability to make antibodies against different pathogens.
A good example of immunological memory is shown in vaccinations. A vaccination against a virus can be made using either attenuated virus, meaning active but weakened virus, or using specific parts of the virus that are not active. Neither attenuated whole virus nor virus particles can actually cause an active infection. Instead, they mimic the presence of an active virus to cause an immune response, even though there are no real threats present: the antigens in the vaccine activate the same immune cells that the actual pathogen would, but without causing you to get sick. So by getting a vaccination, you are exposing your body to the antigen required to produce antibodies specific to that virus, and acquire a memory of the virus, without experiencing illness.
Here’s a recent NPR story that drives home the relevance of vaccination: Measles in Europe
What happens when the immune system doesn’t help keep out invaders?
[From Openstax Biology]
A functioning immune system is essential for survival, but even the sophisticated cellular and molecular defenses of the mammalian immune response can be defeated by pathogens at virtually every step. In the competition between immune protection and pathogen evasion, pathogens have the advantage of more rapid evolution because of their shorter generation time and other characteristics. For instance, Streptococcus pneumoniae (the bacterium that causes pneumonia and meningitis) surrounds itself with a capsule that inhibits phagocytes from engulfing it and displaying antigens to the adaptive immune system. Staphylococcus aureus (a bacterium that can cause skin infections, abscesses, and meningitis) synthesizes a toxin that kills phagocytes after they engulf the bacterium. Other pathogens can also hinder the adaptive immune system. HIV infects helper T cells via their CD4 surface molecules, gradually depleting the number of helper T cells in the body. The depletion of helper T cells inhibits the adaptive immune system’s capacity to generate sufficient responses to infection or tumors. As a result, HIV-infected individuals often suffer from infections that would not cause illness in people with healthy immune systems but which can cause devastating illness to immune-compromised individuals.
Immunodeficiency
Failures in the immune response can allow pathogens or tumor cells to gain a foothold and proliferate to levels that can overwhelm the immune system. Immunodeficiency is the failure, insufficiency, or delay in the response of the immune system, and it may be acquired or inherited. Immunodeficiency can be acquired as a result of infection with certain pathogens (such as HIV), chemical exposure (including certain medical treatments), malnutrition, or possibly by extreme stress. For instance, radiation exposure can destroy populations of lymphocytes and elevate an individual’s susceptibility to infections and cancer. Dozens of genetic disorders result in immunodeficiencies, such as MHC II deficiencies. Rarely, immunodeficiencies can be present from birth, like neutropenia. In Neutropenia, the immune system produces a too few phagocytes, and the immune system fails to prevent blood-born bacterial infections.
Hypersensitivities – Allergy & Autoimmunity
Allergies are an immune reaction that occurs within minutes of exposure to a harmless antigen. The antigen triggers an antibody-mediated immune response. In the US, 20% of the population exhibits symptoms of allergy or asthma, but a whopping 55% test positive against one or more allergens. How does that work? Upon initial exposure to a potential allergen, an allergic individual makes antibodies for the normally benign antigen: antigen presenting cells present the processed antigen to helper T cells, which then stimulate B cells to produce antibodies. This process sensitizes the immune system to a secondary exposure. Upon subsequent exposure to the same allergen, antibodies on white blood cells called mast cells bind the antigen and stimulate release of histamine and serotonin.
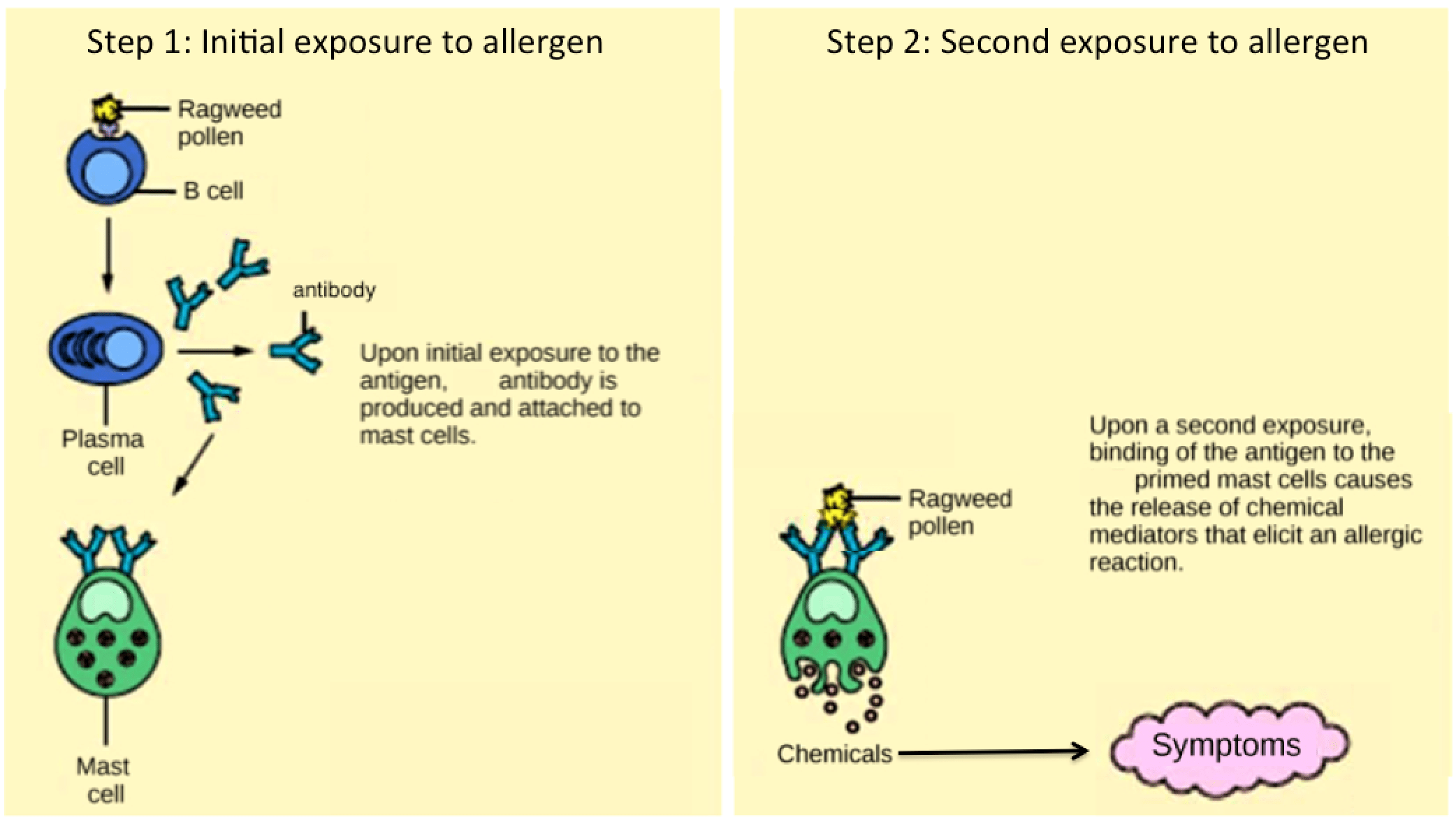
On first exposure to an allergen, an antibody is synthesized by plasma cells in response to a harmless antigen. The antibodies bind to mast cells, and on secondary exposure, the mast cells release histamines and other modulators that affect the symptoms of allergy. (credit: modification of work by NIH)
The effects of an allergic reaction range from mild symptoms like sneezing and itchy, watery eyes to more severe or even life-threatening reactions involving intensely itchy welts or hives, airway contraction with severe respiratory distress, and plummeting blood pressure. This extreme reaction is known as anaphylactic shock. If not treated with epinephrine to counter the blood pressure and breathing effects, this condition can be fatal.
Delayed hypersensitivity is a cell-mediated immune response that takes approximately one to two days after secondary exposure for a maximal reaction to be observed, like contact dermatitis (rash or skin irritation) in response to contact with certain types of jewelry, cosmetics, or chemicals. It also facilitates the immune response to poison ivy and is the reason why the skin test for tuberculosis results in a small region of inflammation on individuals who were previously exposed to Mycobacterium tuberculosis. We use cortisone to treat such responses because cortisone inhibits cytokine production.
Autoimmunity
Autoimmunity is a type of hypersensitivity to your body’s own antigens. About 5% of the US population has some form of autoimmunity. Most types of autoimmunity involve the humoral immune response. Here are some examples:
In myasthenia gravis patients, antibodies target their own muscle cell receptors, preventing muscle contraction. Resulting muscle weakness may include extreme difficultly with both fine muscle control and gross motor functions like walking.
In systemic lupus, a diffuse autoantibody response to the individual’s own DNA and proteins results in various systemic diseases. Lupus may affect the heart, joints, lungs, skin, kidneys, central nervous system, or other tissues, causing tissue damage via antibody binding, complement recruitment, lysis, and inflammation.
Autoimmunity can develop with time, and the causes may be linked to molecular mimicry. Imagine if some of your self antigens are structurally similar to pathogen antigens; antibodies might then recognize self as foreign. As an example, infection with Streptococcus pyogenes (bacterium that causes strep throat) may generate antibodies or T cells that react with heart muscle, which has a similar structure to the surface of S. pyogenes. These antibodies can damage heart muscle with autoimmune attacks, leading to rheumatic fever. Insulin-dependent (Type 1) diabetes mellitus arises from a destructive inflammatory helper T cell response against insulin-producing cells of the pancreas. These patients require injection with insulin that originates from other sources.