Learning Objectives
- Identify and describe functions of key anatomical reproductive structures present in various types of animals, including the spermatheca, the cloaca, the ovary and related structures, and the testes and related structures
- Compare and contrast how and when eggs and sperm are made in meiosis
- Describe roles of hormones in gametogenesis, ovulation, and implantation, comparing which are similar and which are different in male and females
- Explain how various birth control interventions affect reproductive cycles and fertilization
Diversity of Animal Reproductive Anatomy
The information below was adapted from OpenStax Biology43.2
The reproductive structures of many animals are very similar, even across different lineages, in a process that begins with two gametes–eggs and sperm–and ends with a zygote, which is a fertilized egg. In animals ranging from insects to humans, males produce sperm in testes and sperm are stored in the epididymis until ejaculation. Sperm are small, mobile, low-cost cells that occur in high numbers. Females produce an ovum or egg that matures in the ovary. Eggs are large cells that require a substantial investment of time and energy to form, are non-mobile, and are rare relative to sperm numbers. When the eggs are released from the ovary, they travel to the uterine tubes for fertilization (in animals that reproduce via internal fertilization) or are released in the aqueous environment (in animals that reproduce via external fertilization).
The first half of Hank Green’s Crash course video below has a nice summary of these ideas for a diversity of eukaryotes, while the second half of the video introduces the human reproductive anatomy before we take a deeper dive into the structures and functions via dynamic hormonal changes.
For our purposes, all sexual reproducers have females with ovaries that produce large eggs, which subsequently travel down a uterine tube, and males with testes that produce small, plenteous sperm, stored in an epididymus. Of course, beyond this general anatomy, there are some differences in different types of animals:
- In many insects and some mollusks and worms, the female has a specialized sac, the spermatheca, which stores sperm for later use, sometimes up to a year. Fertilization can be timed with environmental or food conditions that are optimal for offspring survival.
- Non-mammal vertebrates, such as most birds and reptiles, have a cloaca, a single body opening for the digestive, urinary, and reproductive systems. Mating between birds usually involves positioning the cloaca openings opposite each other for transfer of sperm from male to female. Ducks are a rare exception, where the males have a penis.
- Mammals have separate openings for digestive, excretory, and reproductive systems in the female, and placental mammals have a uterus where offspring develop.
The remainder of today’s content focus on human reproduction and include structures as well as hormonal control. We will provide a list of the anatomy you need to know and would like you to focus on the hormones and how they work together to support effective reproduction. Hormones are dynamic (changing), so this process can be trickier to understand. Hormonal changes are the center of the fascinating biology of reproduction.
The human female reproductive system
| Organ | Function |
|---|---|
| Ovaries | Produces and develops eggs |
| Fallopian tubes (oviducts) | Transports egg to uterus, acts as site of fertilization |
| Uterus | Supports a developing embryo |
| Cervix | Allows passage between the uterus and the vagina |
| Vagina | Receives penis during intercourse, acts as birth canal, passes menstrual flow |
| Breasts | Produce and deliver milk |
During puberty, the hypothalamus in the brain signals the pituitary gland to produce two hormones, follicle-stimulating hormone (FSH) and luteinizing hormone (LH). In females, FSH and LH stimulate the ovaries to produce the female sex hormones, estrogen and progesterone. This results in the development of secondary sex characteristics (such as breasts) and causes the ovaries to begin producing mature eggs.
Egg release (ovulation) occurs approximately every 28 days as part of a larger process called the menstrual cycle. If an egg is fertilized after ovulation, it attaches to the wall of the uterus and embryonic development begins. If an egg is not fertilized (or a fertilized egg does not attach to the wall of the uterus), the egg and the lining of the uterus are discharged from the body.
Reproductive hormones in females
The control of reproduction in females is complex, and we’ll focus on the basics here. Egg production is controlled by FSH, LH, estrogen, and progesterone.
- FSH stimulates development of egg cells that develop in structures called follicles.
- LH also plays a role in the development of eggs and induction of ovulation.
- Estrogen is the reproductive hormone in females that assists in ovulation and regrowing the lining of the uterus; it is also responsible for the secondary sexual characteristics of females such as breast development.
- Progesterone assists in endometrial re-growth and inhibition of FSH and LH release.
These hormones together regulate the ovarian and menstrual cycles. The ovarian cycle controls the production and release of eggs, while the menstrual cycle governs the preparation and maintenance of the uterine lining. These cycles occur concurrently and are coordinated over a 22–32 day cycle, with an average length of 28 days:
- The first half of the ovarian cycle is the follicular phase. Slowly rising levels of FSH and LH cause the growth of follicles on the surface of the ovary. This process prepares the egg for ovulation. As the follicles grow, they begin releasing estrogens and a low level of progesterone. Estrogen levels increase over the course of the follicular phase as the follicles continue to develop. In the menstrual cycle, menstrual flow occurs at the beginning of the follicular phase when estrogen levels are low (when the follicles are only just beginning to develop); rising levels of estrogen then cause the lining of the uterus to grow, replacing the blood vessels and glands that deteriorated during the end of the last cycle.
- Ovulation occurs just prior to the middle of the cycle (approximately day 14), when the high level of estrogen produced by the developing follicles causes FSH and especially LH to rise rapidly, then fall. The spike in LH causes ovulation: the most mature follicle ruptures and releases its egg. The follicles that did not rupture degenerate and their eggs are lost. The level of estrogen decreases when the extra follicles degenerate.
- Following ovulation, the ovarian cycle enters its luteal phase, and the menstrual cycle enters its secretory phase, both of which run from about day 15 to 28. The cells in the ruptured follicle produce a structure called a corpus luteum, which in turn produces estrogen and progesterone. The progesterone facilitates the regrowth of the uterine lining and inhibits the release of further FSH and LH. The uterus becomes prepared to accept a fertilized egg, should fertilization occur. The inhibition of FSH and LH prevents any further eggs and follicles from developing, while the progesterone is elevated. The level of estrogen produced by the corpus luteum increases to a steady level for the next few days. Estrogen enhances the effects of progesterone.
- It takes about seven days for an egg to travel through the fallopian tube from the ovary to the uterus, and fertilization occurs in the fallopian tube.
- If no fertilized egg is implanted into the uterus, the corpus luteum degenerates and the levels of estrogen and progesterone decrease. The lining of the uterus begins to degenerate as the progesterone levels drop, initiating the next menstrual cycle. The decrease in progesterone also allows the hypothalamus to trigger the pituitary to release FSH and LH and start the cycles again.
- If a fertilized egg implants in the endometrial lining of the uterine wall, the embryo produces a hormone called hCG that maintains the corpus luteum. The ovary continues to produce progesterone at high levels, and the menstrual cycle is arrested for the duration of the pregnancy. Because hCG is unique to pregnancy, it is the hormone detected by pregnancy tests.
The figure below visually compares the ovarian and uterine cycles as well as the hormone levels controlling these cycles.
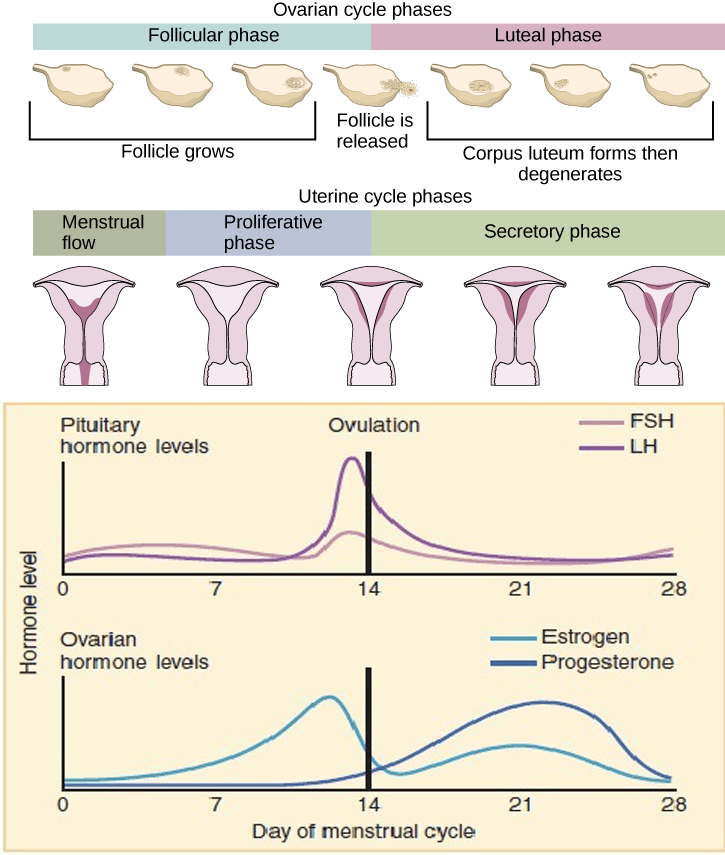
Rising and falling hormone levels result in progression of the ovarian and menstrual cycles. Image credit: modification of work from OpenStax Biology and OpenStax Anatomy and Physiology; modification of work by Mikael Häggström)
The human male reproductive system
| Organ | Location | Function |
| Scrotum | External | Carry and support testes |
| Penis | External | Deliver urine, copulating organ |
| Testes | Internal | Produce sperm and male hormones |
| Seminal Vesicles | Internal | Contribute to semen production |
| Prostate Gland | Internal | Contribute to semen production |
| Epididymis | Internal | Sperm storage |
In response to signals from the hypothalamus that begin at the onset of puberty in males, the pituitary gland produces FSH. FSH enters the testes to begin facilitating spermatogenesis, which is the production of sperm cells (gametes) by meiosis. LH, made by the pituitary, also enters the testes to stimulate the production and release of testosterone into the blood. Testosterone stimulates spermatogenesis as well as the development of male secondary sex characteristics that include a deepening of the voice, the growth of facial, axillary, and pubic hair, and the beginnings of the sex drive. When sperm counts get too high (over about 20 million/ml), rising testosterone levels act on the hypothalamus and pituitary gland to inhibit the release of FSH and LH. The inhibition causes spermatogenesis to slow down until proper levels are again achieved.

Hormonal regulation of human male reproduction. Image credit: Brian Hammer.
Sperm production is largely controlled by the major male hormone, or androgen, called testosterone.
- FSH facilitates meiosis in the testes.
- LH stimulates testosterone production.
- Testosterone is the reproductive hormone in males for secondary sexual characteristics of males such as deepening of the voice, body hair, and sex drive.
This video provides a concise overview of the anatomy and function of the male reproductive system:
How and when are gametes made?
As you’ve just seen in the two videos the production of sperm and eggs takes place through the process of meiosis, which we learned about in an earlier reading. There are some big differences between the processes to make eggs versus sperm:
- When gametes start to form: Egg production begins during embryonic development (before birth), then is arrested during meiosis until puberty; sperm production does not begin until puberty
- When gametes finish being made: Egg production is not actually completed until after fertilization (!), while sperm production is complete prior to ejaculation
- How many gametes are made from a gamete stem cell: Egg production results in only a single egg from each egg stem cell; sperm production results in four sperm from each sperm stem cell.
- Rate of production: Once an individual enters puberty, sperm production is continuous in a “conveyor belt” process; egg production occurs one-at-a-time at each menstrual cycle.
Contraception and Birth Control
The information below was adapted from OpenStax Biology 43.5
Methods of contraception to prevent pregnancy have varying probabilities of success. In the diagram below, the failure rate is the given as the percent of women who become pregnant during the first year of use of that method.

Source: Center for Disease Control and Prevention – https://www.cdc.gov/reproductivehealth/UnintendedPregnancy/PDF/effectiveness_of_contraceptive_methods.pdf, Public Domain, https://commons.wikimedia.org/w/index.php?curid=27189006
Work through the methods in this diagram to determine the most effective strategies for preventing pregnancy. Methods in combination, such as spermicidal chemicals and barrier, prevent pregnancy more effectively than do the methods when used separately.
What causes failure? Not all sperm are in the ejaculate, so without a barrier, a some sperm may still enter the vagina. Hormonal methods vary in success by hormone delivery method. A method not pictured is emergency contraception, also known as “Plan B.” This hormone-based method of contraception works against the egg and the sperm simultaneously, and before the fertilization occurs.
This video provides a quick overview of hormone-based birth control, with emphasis on emergency contraception:


