Learning Objectives
- Identify and differentiate between the functions and actions of the innate versus adaptive immune responses, and know that only jawed vertebrates have an adaptive immune system.
- Describe and differentiate between the cell-mediated and humoral responses of the adaptive immune system.
- Describe the role of antibodies, antigens, and antigen presenting cells.
- Compare and contrast B cell antibodies and T cell receptors as antigen receptors.
- Explain immune specificity, memory, and response rate upon second infection in terms of selection of B cells and T cells.
- Explain how the adaptive immune system works in response to a vaccination to create immunity in the host, including the names of the immune system cells and how they interact with each other.
- Recognize public health implications of decreased vaccination rates.
We, and all large animals, are large bags of warm meat and broth, a rich food source not just for predators with jaws and claws, but also for the even more deadly, and ubiquitous, microbial and viral pathogens. We live because our immune cells are able to kill or neutralize these invisible predators. What is even more remarkable is that our immune cells evolve repeatedly during our lifetime. Within weeks, they can evolve and adapt to fight pathogens never previously seen by that individual or even previously encountered in human evolutionary history. How does this remarkable immune system work?
Innate versus adaptive immunity
All organisms, from bacteria to trees to worms and humans, have innate immune defenses. These range from physical barriers to anti-microbial chemicals. But only jawed vertebrates have evolved the complex, adaptive immune system featuring antibodies and killer cells that recognize billions of different pathogen molecules with high specificity.
Innate immunity is non-specific
All organisms have some type of innate immunity, whether it be a cell membrane, skin or scales, and mucous membranes to keep the non-self separated from the self. Once this barrier is broken, the body mounts an inflammatory response: fever, chemical signals, inflammation. Certain white blood cells produce histamines to cause swelling, call in other types of white blood cells, including neutrophils, which attack invaders and then die, producing pus.
The second line of inflammatory response in the white blood cells’ defense of the organism are phagocytic cells, which are cells that literally engulf and digest other cells, and natural killer cells, which are able to trigger apoptosis to kill body cells infected with viruses or producing tumours.
Sometimes, the innate immune response is overwhelmed by the sheer number of invaders. In these cases, it triggers an increase in body temperature, causing a fever, which makes the invading cells as unhappy as it makes you feel.
Two arms of the adaptive immune system
The adaptive immune system has two distinct approaches to destroying pathogens: the humoral response and the cell-mediated response. The humoral response works via B cells that produce antibodies, which bind to and effectively neutralize an invader so that it can’t infect a cell. The cell-mediated response works via cytotoxic (cell-killing) T cells that kill any body cells infected with the pathogen. B cells (and to some extent, cytotoxic T cells) only become activated after they interact with a third type of cell, called helper T cells.
Adaptive immune system has specificity and memory
The adaptive immune system takes some time, 1-2 weeks, to mount a full-fledged response to any new pathogen or biological macromolecule that it encounters for the first time. However, the second time it sees the same pathogen or macromolecule, it mounts an immediate, even stronger response. Both the response and the memory are highly specific for the pathogen or macromolecule.
The specificity of the adaptive immune system arises from its antigen receptors: T-cell receptors and antibodies. Anything that binds to an antigen receptor is defined as an antigen, short for antibody generator.
T cells and B cells generate millions of different antigen receptors, hopefully one that matches every invader that might attack
T cells and B cells are lymphocytes, types of white blood cells, that are able to recognize foreign (non-self) antigens. T cells display T-cell receptors on their cell surface, while B cells display antibodies attached to the cell surface. There are two different types of T cells: helper T cells and cytotoxic T cells. Helper T cells are essential intermediaries that activate both cytotoxic T cells and B cells. Activated cytotoxic T cells act to kill body cells that are infected with pathogens. Activated, B cells divide and differentiate (mature) into plasma (or effector) cells that secrete large amounts of free antibody molecules that circulate in the blood and lymph systems, looking for invaders.
Immune responses begin with antigen processing and presentation to helper T cells
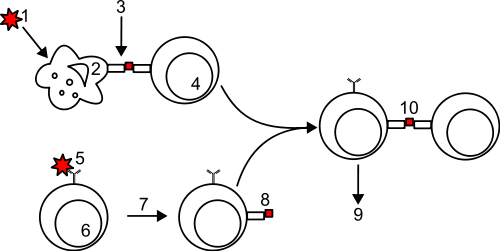
Although it’s clear after the fact that antigens (1 on the diagram below) are invaders, the immune system has a safeguard to mounting an immune response: every antigen undergoes processing before it evokes an immune response. Antigens are processed by professional antigen presenting cells (APCs) that eat the suspected foreign invader and then display bits of the invader on the cell surface, attached to their Major Histocompatibility (MHC) proteins.The most important professional antigen presenting cells are macrophages, dendritic cells, and B cells. Any substance that cannot be 1) processed and 2) displayed on MHC II proteins cannot provoke an immune response.
Helper T cells are activated when their T-cell receptor recognizes the antigen presented by an antigen presenting cell. Upon activation, helper T cells divide to form both activated helper T cells and long-lived memory helper T cells. In this course, we expect you to be able to interpret this labeled diagram to explain how the adaptive immune system is activated by a pathogen.
The diagram above shows the numbered steps to activate antibody production by adaptive immune system, with two processes that occur in tandem and result in the same outcome:
- An antigen or pathogen is eaten by an antigen-presenting-cell (APC)
- The APC processes the antigen/pathogen, producing peptide fragments (small bits of proteins)
- The APC presents the peptide fragments on its surface by binding them to its MHC molecules
- A specific helper T cell recognizes the peptide-MHC complex via its T-cell receptor and is activated to divide
- At the same time as steps 1-4, A B cell binds the antigen via its cell surface antibody
- The B-cell internalizes (“eats”) the antigen-antibody complex and processes it into peptide fragments
- The B cell presents processed peptide on its MHC molecules
- A specific, activated helper T cell recognizes the peptide-MHC complex
- The helper T cell activates the B cell
- The B cell divides and produces plasma cells that secrete lots of antibody molecules
- NOT SHOWN: activated helper T cells also help activate specific cytotoxic T cells, which then seek out and destroy any body cells that are infected with the pathogen. Cytotoxic T cells can also be activated by interacting directly with APCs.
B cells recognize antigens via cell-surface antibodies
B cells are responsible for the humoral immune response of antibody molecules working outside of cells in the blood, lymph, and intercellular matrix. B cells recognize and bind antigens via their cell surface antibodies. They eat, process, and present fragments of the antigen on their cell surface MHC proteins. If these are recognized by a previously activated helper T cell, the helper T cell stimulates the B cell to divide. When the B cell divides, it forms both plasma cells that secrete vast amounts of free moving antibodies and long-lived memory B cells.
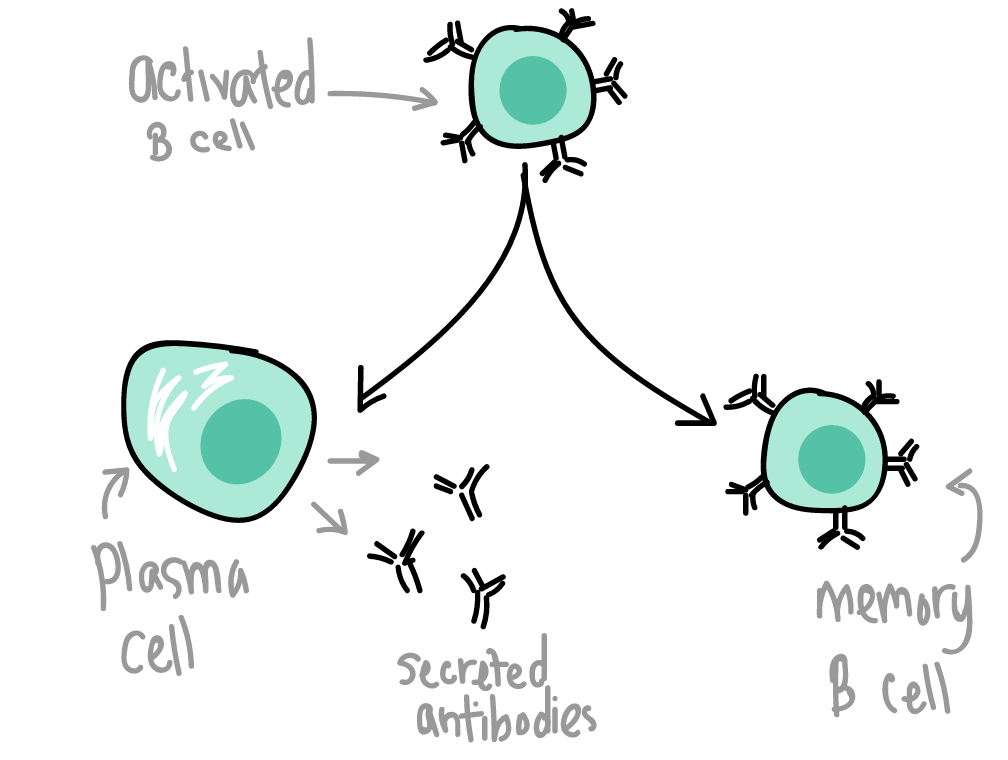
[Image credit: Khan Academy]
Killer T cells recognize and kill body cells that present foreign antigens
The cell-mediated branch of the immune system relies on cytotoxic T cells. Cytotoxic T cells are the internal security forces. Cytotoxic T cells look for cells that are presenting non-self or altered peptides on MHC molecules. Cytotoxic T cells can be activated by both helper T cells and APCs.
Most body cells display MHC proteins that show fragments of the proteins that the cells are making. If they are healthy cells, they are making normal proteins and the immune system ignores them (“self” proteins). But invaded or sick cells display unusual protein fragments: virus-infected cells will present fragments of viral proteins, and cancerous cells will present fragments of tumor proteins, which are mutated versions of normal cellular proteins.
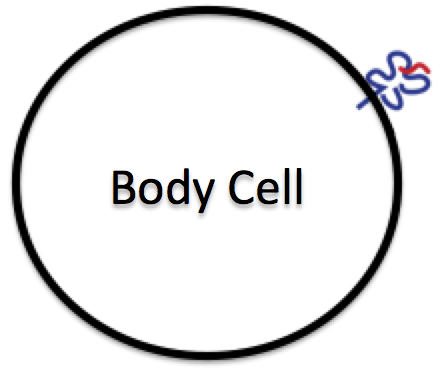
Body cell with an MHC protein (blue) displaying a fragment of an antigen (red).
Cytotoxic T cells whose receptors recognize these foreign or tumor fragments bound to the MHC become activated; they kill the virus-infected or cancerous cell by inducing apoptosis. Cytotoxic T cells are very precise in what they recognize as foreign, so they also kill cells that express a different MHC allele than the host–this is the basis for tissue graft rejection, and why it is so tricky to find a matching donor for tissue and organ transplants. The donor must have MHC alleles that match the recipient.
Clonal selection of T-cells and B-cells lead to specific immune responses and long-term immune memory
When B and T cells are young, their DNA variation is reduced so that they can produce a specific antigen. That means that B and T cells do not contain a complete genome! Any one of these cells would be poor choices for cloning. Taken together, each can recognize one of millions of different invaders. When an invader shows up and activates the adaptive immune response, the lymphocytes that recognize that invader replicate and increase in frequency, producing additional memory cells for that invader. So, the adaptive immune system operates on evolutionary principles of selection! And, the next time that the same pathogen enters the body, it will be recognized much more quickly, and the immune response will be much stronger:

Antigen A is given once to generate a primary response and later to generate a secondary response. When a different antigen is given for the first time, a new primary response is made. Image credit: OpenStax Anatomy & Physiology
Here’s Hank Green’s Crash Course overview of the innate and adaptive immune responses:
What are vaccines and how do they work?
[From Khan Academy]
Because the adaptive immune system can learn and remember specific pathogens, it can provide long-lasting defense and protection against recurrent infections. When the adaptive immune system is exposed to a new threat, the specifics of the antigen are memorized so we are prevented from getting the disease again. The concept of immune memory is due to the body’s ability to make antibodies against different pathogens.
A good example of immunological memory is shown in vaccinations. A vaccination against a virus can be made using either attenuated virus, meaning active but weakened virus, or using specific parts of the virus that are not active. Neither attenuated whole virus nor virus particles can actually cause an active infection. Instead, they mimic the presence of an active virus to cause an immune response, even though there are no real threats present: the antigens in the vaccine activate the same immune cells that the actual pathogen would, but without causing you to get sick. So by getting a vaccination, you are exposing your body to the antigen required to produce antibodies specific to that virus, and acquire a memory of the virus, without experiencing illness.
Here’s a recent NPR story that drives home the relevance of vaccination: Measles in Europe
What happens when the immune system doesn’t help keep out invaders?
[From Openstax Biology]
A functioning immune system is essential for survival, but even the sophisticated cellular and molecular defenses of the mammalian immune response can be defeated by pathogens at virtually every step. In the competition between immune protection and pathogen evasion, pathogens have the advantage of more rapid evolution because of their shorter generation time and other characteristics. For instance, Streptococcus pneumoniae (the bacterium that causes pneumonia and meningitis) surrounds itself with a capsule that inhibits phagocytes from engulfing it and displaying antigens to the adaptive immune system. Staphylococcus aureus (a bacterium that can cause skin infections, abscesses, and meningitis) synthesizes a toxin that kills phagocytes after they engulf the bacterium. Other pathogens can also hinder the adaptive immune system. HIV infects helper T cells via their CD4 surface molecules, gradually depleting the number of helper T cells in the body. The depletion of helper T cells inhibits the adaptive immune system’s capacity to generate sufficient responses to infection or tumors. As a result, HIV-infected individuals often suffer from infections that would not cause illness in people with healthy immune systems but which can cause devastating illness to immune-compromised individuals.
Additional Resources (optional):
The video below provides a very nice 6-minute overview of the immune response. It does briefly cover the complement system, which is not covered in this course: